Ot Feeding Strategies in Elderly Population
The incidence and impact of malnutrition in older people is underestimated. The best option for treating malnutrition is to enhance normal eating and drinking. A "Food First" approach encourages eating frequent, small, high energy and protein meals and snacks. Nutritional supplements for weight gain are generally not required unless body weight is unable to be maintained with a normal balanced diet, or if food cannot be eaten safely.
- Changes to the funding of oral nutritional supplements
- Defining malnutrition
- How do we detect under-nutrition?
- Malnutrition Universal Screening Tool (MUST)
- Nutrition support strategies
- References
In this article
In this article ![]()
View / Download pdf version of this article
Key concepts
- The incidence and impact of malnutrition in elderly people is underestimated
- Routine screening for malnutrition should be implemented for people in at risk groups
- "Food First" – eating small but frequent, high energy, high protein snacks and meals – is the first treatment option for elderly people who are malnourished
- Use of oral nutritional supplements (ready-made sip feeds or powders which are mixed with water or milk) is generally not recommended until a Food First approach has been trialled
- Nutrition support is recommended for malnourished people who are unable to maintain body weight by food intake alone
- Oral nutritional supplements are a top-up to food intake rather than a replacement – they should be given between meals, not at meal times
Changes to the funding of oral nutritional supplements
PHARMAC has recently made a number of changes to the access and funding of oral nutritional supplements, including powders for reconstitution and ready-made liquids. These changes include:
- Reducing the funding of ready-made liquids to the level of powder alternatives
- Widening access to those who can initiate funding (vocationally registered general practitioners can now make initial Special Authority applications)
- Restricting funding to people who are malnourished or who have one of a number of listed specific indications which places them at high risk of malnourishment
- Emphasising "Food First" and regular review of patients
Background to the recent funding changes
In New Zealand, use of ready-made liquid supplements has been increasing steadily. Expenditure on standard adult oral and enteral products was $6.7 million in 2008/09 with annual growth of 13%. Of this, $5.7 million was for ready-made liquids, e.g. Ensure Plus and Fortisip (see graph Allergy to cows' milk protein and the appropriate use of infant formula).
In the United Kingdom there has been concern regarding the treatment approach to malnutrition in elderly people. This has resulted in the formulation of treatment guidelines emphasising the provision of nutritional supplementation to only those who are malnourished or at a high risk of malnourishment, an emphasis on the use of first line dietary advice (Food First), and regular patient reviews
Defining malnutrition
Malnutrition is both a "cause and a consequence of ill-health".1 The term malnutrition can apply to various states – under-nutrition, over-nutrition or deficiencies of specific nutrients. This article will concentrate on under-nutrition, and the term malnutrition when used will refer to this state. More specifically, malnutrition in this context refers to a deficiency in protein and energy, with or without micronutrient deficiencies. Such deficiencies are associated with a decline in body functioning and clinical outcome. The consequences of malnutrition are physiological, biochemical and psychological. They include reduced immunity, delayed wound healing and decreased muscle strength, which in turn have detrimental effects on recovery and rehabilitation. The psycho-social impact of malnutrition is also significant with changes in mood, attitude, self esteem and reduced socialisation.1,2,3
Prevalence of under-nutrition
| Estimates of prevalence of under-nutrition in elderly people: | |
| Prevalence | Type of population |
| Over 10% | Non-institutionalised elderly people1 |
| 10 – 50% | Hospitalised for acute illness4 |
| 10 – 70% | Long care units or nursing homes1,5 |
Causes of malnutrition
The "anorexia of ageing"6,7
Appetite and food intake often decline with ageing. Older people tend to be consistently less hungry than younger people, eat smaller meals, have fewer snacks between meals and also eat more slowly.8 Between age 20 and 80 years, there is on average, a decrease in energy intake of approximately 30%. When this decline in energy intake is more than the decrease in energy use that is also normal with ageing, then there is loss of weight.8
Most people lose weight as they age, but the amount lost is variable and those that are already lean, also lose weight. The problem with this weight loss is that it is not only unwanted adipose tissue that is lost but lean skeletal muscle.9 The loss of lean tissue is associated with reductions in muscle function, bone mass and cognitive function, anaemia, dysfunction of the immune system, slow wound healing and recovery from surgery, and consequentially an increase in both morbidity and mortality.8,9 Although lean muscle can be regained in younger people this is often not the case for elderly people. This means that being underweight becomes more of a health problem in older age, than being overweight.
Increasing age has several effects on gastrointestinal function. Secretion of gastric acid, intrinsic factor and pepsin is decreased, which then reduces the absorption of vitamin B6, B12, folate, iron and calcium. Other gastrointestinal problems such as gastritis and gastrointestinal cancers can reduce nutritional status.10
A hypermetabolic state where there is increased resting energy use can be caused by acute respiratory or urinary infections, sepsis, cirrhosis of the liver, hyperthyroidism and the hyperactive state found in some people with dementia or Parkinson's disease.10 Chronic obstructive pulmonary disease (COPD) can cause anorexia and physical problems related to shortness of breath (see here).
In addition to the "anorexia of ageing", there are physical, social, cultural, environmental and financial reasons for an inadequate diet.1,8
Impaired intake
Poor appetite: illness, pain or nausea when eating, depression or anxiety, social isolation or living alone, bereavement or other significant life event, food aversion, resistance to change, lack of understanding linking diet and health, beliefs regarding dietary restrictions, alcoholism, reduced sense of taste or smell.
Inability to eat: confusion, diminished consciousness, dementia, weakness or arthritis in the arms or hands, dysphagia, vomiting, COPD, painful mouth conditions, poor oral hygiene or dentition, restrictions imposed by surgery or investigations, lack of help while eating for those in hospitals and rest homes.
Lack of food: poverty, poor quality diet (home, hospital or rest home), problems with shopping and cooking, ethnic preferences not catered for, particularly in hospitals and rest homes.
Medicines: medicines can alter nutritional status in numerous ways, e.g. anorexia, decreased or altered taste, dry mouth, confusion, gastrointestinal disturbance including nausea, vomiting, diarrhoea, constipation, dyspepsia. Incorrect use of medicines may also cause problems, e.g. hypermetabolism with thyroxine and theophylline.10
Impaired digestion and/or absorption: Medical and surgical problems affecting stomach, intestine, pancreas and liver, cancer, infection, alcoholism
Altered requirements: Increased or changed metabolic demands related to illness, surgery, organ dysfunction or treatment.
Excess nutrient losses: Vomiting, diarrhoea, fistulae, stomas, losses from nasogastric tube and other drains.
Illness related Malnutrition: Some disease states also increase the risk of malnutrition. For example chronic respiratory, gastrointestinal, liver and kidney diseases, cancer, HIV, AIDS, stroke and surgery.1
Surgery: The metabolic changes caused by surgery, the increased demands required for successful healing, sepsis and the stress of the surgical procedure itself, all increase energy needs.11 To supply this energy, protein stored as muscle is broken down and amino acids released. A septic state will increase this muscle breakdown further. Nutritional requirements must meet these increased needs. Furthermore, patients may already be malnourished due to the illness that led to their surgery.
Once discharged, there will be ongoing higher nutritional needs during the recovery phase, although muscle lost may never be regained. Oral nutritional supplements may be useful during the recovery period, particularly if there are modifications to dietary intake as a consequence of the surgery, e.g. texture modification, low residue diet.
Cancer: People with cancer are often malnourished. Physical and metabolic changes can be compounded by social and psychological problems.12 Treatment adverse effects such as taste changes, nausea or swallowing difficulties also result in a reduced food and nutrient intake. Cancer may result in cachexic syndrome which is a state of complex metabolic changes associated with anorexia, progressive weight loss and depletion of reserves of adipose tissue and skeletal muscle. Weight loss adversely affects treatment tolerance and survival outcomes.
Nutritional advice tailored on an individual basis should be given at an early stage to help prevent nutritional deficiencies.13 Loss of appetite, pain, nausea and vomiting all contribute to poor oral intake. Prednisone may be used to stimulate appetite, but its effect tends to be short lived.14
Oral nutritional supplements can be beneficial when a normal balanced diet cannot be tolerated. These supplements help prevent malnutrition but eventually cannot halt the cachexic state associated with many end-stage cancers.
Chronic Kidney Disease (CKD) 15 Nutritional requirements for people with CKD vary widely. In general, they require a diet that promotes adequate nutrition, minimises biochemical abnormalities and delays the progression of CKD. In later stages of CKD appetite is often poor and there is a high risk of malnutrition.
Guidance should be given to ensure the protein intake meets the recommended daily intake for the patients' age and gender and adequate energy is consumed. Micronutrients such as potassium and phosphorous should only be restricted if blood levels are elevated. The aim of treatment is to prevent malnutrition.
People requiring haemodialysis have some differing needs – they require 1.2 – 1.4 g/kg/day of protein due to losses in the dialysate. Some people may require adjustment of micronutrient intake, but this is dependent on the individual's clinical and biochemical profile.
There are specialised renal nutritional supplements available on the Pharmaceutical Schedule. These are indicated for patients requiring volume and potassium restrictions. For many patients, standard oral nutritional supplements will be suitable in the first instance.
How do we detect under-nutrition?
The onset of nutritional problems is often gradual and therefore hard to detect. However, features found in the history and examination may help identify those at risk. People can present with a variety of problems that may be vague or non-specific. Patients may report reduced appetite and energy and have altered taste sensation and changes to their normal bowel habit.1 Clinical features that may suggest under nourishment include low body weight, fragile skin, wasted muscles, recurrent infections and impaired wound healing.1
A malnourished state is defined as any of the following:1
- BMI < 18.5 kg/m2
- Unintentional weight loss > 10% within the last three to six months
- BMI < 20 kg/m2 and unintentional weight loss > 5% within the last three to six months
| % weight loss = | original weight - current weight | x 100 |
| current weight |
| BMI = | weight(kg) |
| height(m)2 |
Screening for malnutrition risk
In many cases clinical judgment is sufficient to diagnose under-nutrition. However, not everyone who is malnourished is thin. Objective classification of a patient's risk of malnutrition assists clinical decision making. A validated and reliable nutrition screening tool is the first step in identifying at risk patients.
NICE clinical practice recommendations for nutrition screening1
Screening should take place for:
- All patients on admission to hospital
- All hospital outpatients at their first appointment
- All people in care homes on admission
- All people on registration at GP surgeries
- Upon clinical concern, e.g. patients with unintentional weight loss, prolonged intercurrent illness or poor wound healing.
Screening should also be considered at other opportunities, e.g. health checks, influenza injections, and repeated regularly for people in recognised risk groups.
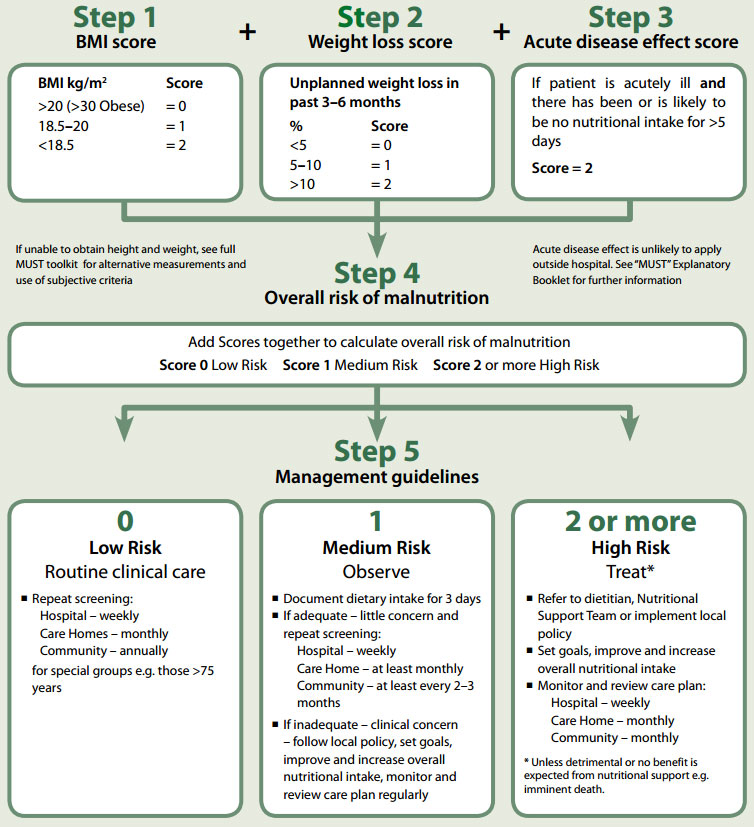
Nutrition screening is defined as a quick and simple evaluation that detects the risk of malnutrition and guides implementation of a clear action plan.1,16 The NICE guidelines recommend the Malnutrition Universal Screening Tool (MUST) which aggregates scores for BMI, unintentional weight loss (over three to six months) and an acute illness or lack of adequate food for more than five days.1
Malnutrition Universal Screening Tool (MUST)
Malnutrition Universal Screening Tool (MUST)
MUST was originally designed for residential and community settings, however, it has now been validated in the acute setting, allowing screening to occur across the continuum of care. It takes on average three to five minutes to complete and includes clear treatment plans depending on the level of risk identified (Figure 1).
 Further information and instructions on the use of the MUST toolkit are available from: www.bapen.org.uk
Further information and instructions on the use of the MUST toolkit are available from: www.bapen.org.uk
The full MUST toolkit includes tables that allow scoring of BMI and % weight loss without having to calculate the individual indices. These can be printed for clinical use. There is also a MUST calculator available to further speed up the screening process.
The complete MUST toolkit is available for download from:
www.bapen.org.uk/pdfs/must/must_full.pdf
An on-line calculator for MUST is available from:
www.bapen.org.uk/must-calculator.html
Figure 1: The MUST screening tool (from www.bapen.org.uk)
| All risk categories: | Obesity: |
|
|
Re-assess subjects identified at risk as they move through care settings
See The 'MUST' Explanatory Booklet for further details and The 'MUST' Report for supporting evidence.
Laboratory testing
Laboratory testing is not useful for diagnosing malnutrition, however, some tests may be required to detect specific deficiencies such as iron, folate and vitamin B12.1,10 Albumin has been suggested in the past as a marker of nutritional status but it is now regarded as unhelpful due to the fact that it can be altered by clinical conditions such as dehydration and inflammation.17
Re-feeding Syndrome
Re-feeding syndrome occurs when nutrition support is re-introduced too quickly after a period of significantly reduced intake or starvation. The subsequent change from fat to carbohydrate metabolism causes alterations in electrolyte levels, such as hypophosphataemia, hypokalaemia and hypomagnesaemia. Thiamine levels may also be reduced.18
NICE recommends that people who have eaten little or nothing for five or more days have nutrition support introduced slowly, at a rate of 50% of requirements. Patients at high risk of re-feeding syndrome should be managed by a team who has expert knowledge of nutritional requirements and care.1
Patients at high risk of re-feeding syndrome1
One or more of the following:
- BMI less than 16 kg/m2
- Unintentional weight loss greater than 15% within the last three to six months
- Little or no nutritional intake for more than ten days
- Low levels of potassium, phosphate or magnesium prior to feeding
Two or more of the following:
- BMI less than 18.5 kg/m2
- Unintentional weight loss greater than 10% within the last three to six months
- Little or no nutritional intake for more than five days
- A history of alcohol misuse or taking medicines including insulin, chemotherapy, antacids or diuretics
Nutrition support strategies
Nutrition support is not limited to providing supplements in the form of oral nutritional supplements (ready-made liquids or powdered sip feeds) or enteral feeding. The first step should always be to maximise an individual's nutritional intake from regular food and drink, often termed "Food First". The Food First approach includes increasing the frequency of eating, maximising the nutrient and energy density of food and drink and fortifying food with the addition of fats and sugars. Strategies to optimise adequate oral nutrition are summarised in Table 1.
Table 1: Ways to optimise oral nutrition in elderly people10,19
| Problem | Solution |
| Loss of appetite |
|
| Chewing problems |
|
| Swallowing difficulties |
|
| Fatigue or difficulty obtaining or preparing food |
|
| Mobility problems |
|
| Chronic pain |
|
| Social isolation, depression |
|
In some situations a Food First approach can be sufficient to correct malnutrition outcomes (see "Practical food suggestions").5 For patients who are at very high risk of malnutrition or for whom first-line dietary measures are not sufficient, oral nutritional supplements should be considered in combination with the Food First approach.1,16
Practical food suggestions for people who are malnourished
Healthy eating guidelines promote low fat and low sugar food choices. Patients who are malnourished or losing weight unintentionally, however, must rely on fat and sugar as concentrated sources of calories. The benefit of energy dense foods in these circumstances should be explained to patients and carers to assist compliance. Ideally fats should be heart healthy (oils, margarines, seeds and nuts) but with the priority being to ensure an energy dense intake. Calories from butter, cream, full fat milk and cheese can be utilised.
General suggestions for a Food First approach may include:
- Three small meals with snacks in-between every day
- Two courses for each of the three meals (see below for ideas)
- Add oil, butter, margarine, cream, cheese, dressings, sauces, sugar, honey and spreads to meals and snacks to boost energy intake
- Choose nourishing fluids such as milky drinks, soups or fruit juice instead of water or tea
- Make dessert a regular option rather than a treat
Meal and snack suggestions
- Breakfast:
- Porridge made with milk plus added cream and sugar, followed by toast with liberal amounts of butter or margarine and spreads
- Scrambled eggs with added cheese and bacon followed by yoghurt and fruit
- Light meal
- Thick milk based soup with a protein (meat, egg, cheese or canned fish) and salad filled sandwich or cheese on toast
- Baked beans on toast with added grated cheese followed by dessert
- Main meal
- Meat, fish , chicken or eggs and include potato, rice or pasta, vegetables or salad with added butter/margarine and grated cheese, dressings, gravies or sauces
- If tolerated, use high fat cooking methods such as roasting or frying
- Dessert
- Custard, ice-cream, instant puddings, mousses or yoghurt with fruit and cream
- Milk puddings such as creamy rice, sago or baked custards
- Ready-made baked or sponge puddings with fruit plus cream or ice-cream
- Snacks
- Crackers and cheese, hummus, cottage cheese, cream cheese or dips
- Scones, pikelets, english muffins, crumpets or toast with liberal spreads
- Dried fruit and nuts (with a little chocolate if enjoyed)
- Protein filled sandwiches
- Sweet muffins, cakes and pastries
Other beneficial products available in supermarkets include Complan, Vitaplan and Up & Go. These products are not nutritionally complete and should not be used as a sole source of nutrition. They can, however, be used as part of the Food First approach as the overall emphasis for these patients should be eating foods high in calories and protein.
 Right click here, save target as... to download these suggestions in a PDF.
Right click here, save target as... to download these suggestions in a PDF.
Oral nutritional supplements
Oral nutritional supplements are nutritionally complete liquid supplements that contain a mix of macro and micronutrients. These products are available from pharmacies in:
- A powder form which is reconstituted with water or milk to make 1 kcal/mL or 1.5 kcal/mL liquids – brands include Ensure powder and Sustagen Hospital Formula*>
- Ready-mixed liquid forms (often referred to as sip feeds) – brands include Ensure Plus and Fortisip
Evidence that oral nutritional supplements improve health outcomes is limited. A systematic (Cochrane) review of 62 trials, updated in 2009, concluded that there was evidence of small consistent weight gain following the use of oral nutritional supplements and that for undernourished patients mortality is possibly reduced.3 In addition, there was greater evidence of a reduction in complications compared to previous reviews but the reviewers noted that the data was limited and of poor quality. A further review of dietary advice for illness related malnutrition in adults could not clearly define whether dietary advice or supplements provided better outcomes.20 The reviewers concluded that nutritional intervention (oral nutritional supplement plus other dietary measures) was more effective than no intervention on enhancing short term weight gain but whether survival or morbidity are improved remains uncertain. All reviews agree that oral nutritional supplements are useful means of increasing protein, energy and micronutrient intake when used appropriately and as part of a combination of nutrition support strategies.1,3,16
The success of oral nutritional supplements can be limited by a lack of compliance often due to low palatability, adverse effects, e.g. nausea and diarrhoea, and by cost.16 Some studies have shown that there can be a decrease in the consumption of normal foods when oral nutritional supplements are given,16,21 whereas other studies found no effect on appetite.22 Wastage of up to 35% of these products is also reported.23
Best results are seen when people are offered a variety of different flavours and consistencies and also when the temperature at which the products are consumed is varied.16 Oral nutritional supplements should be given between meals, not at meal times and there is some evidence of improved adherence if administered in small regular doses similar to a medicine.5 They are not usually intended as a food replacement but as a supplement.
As part of clinical monitoring, prescribers should check that patients are using oral nutritional supplements appropriately, as a top up to their food intake rather than a replacement. Ensure patients are clear about the role of oral nutritional supplements in their overall nutritional care.
After trying Food First, oral nutritional supplements should be considered where a patient has been identified at medium to high risk of malnutrition, ideally in combination with Food First. The prescription should be based on the gap between the patient's estimated requirements and how much they are managing orally. The need for continuation of an oral nutritional supplement should be monitored regularly and adjusted as malnutrition risk reduces.1,5
Considering prescription of oral nutritional supplements
Vocationally registered medical practitioners are now able to make initial applications for Special Food Special Authorities. It is intended that dietitians will also be able to make applications in the near future. The eligibility criteria for Special Authorities give clear guidance on who should be considered for oral nutritional supplements. The reduced time span of initial applications encourages regular monitoring and evaluation of continuation of oral nutritional supplements.
The evaluation pathway is summarised in Figure 2.
Figure 2: The evaluation pathway summary
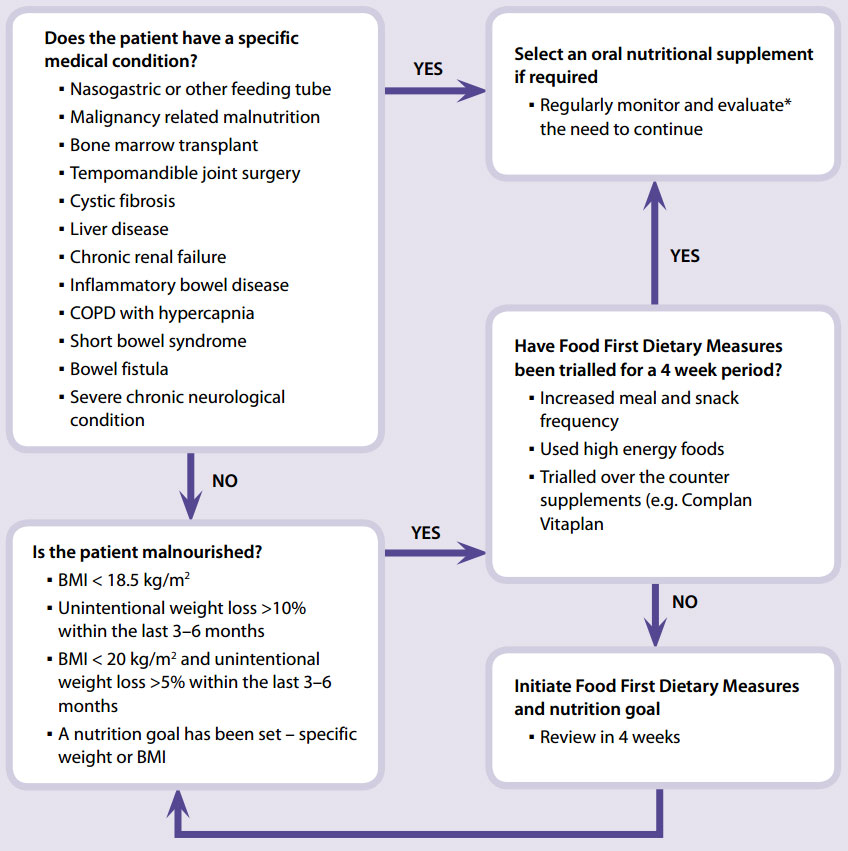
* Monitoring and evaluation considerations may include:
- Is the patient using the supplement? Is there any wastage?
- Is the supplement an addition to food or is it replacing food?
- Changes in weight – is this being recorded?
- Could the patient be encouraged to adopt a diet that meets their nutritional needs, through reiteration of the Food First approach?
- Is there a plan in place to gradually replace use of the supplement with a regular diet?
- Does the patient understand the supplementary role of oral nutritional supplements? Do they require additional ideas or tips on how best to maximise compliance? E.g. recipes, timing in relation to other food and drinks.
Suitable oral nutritional supplements for patients who have been identified at risk of malnutrition
Points for consideration:
- Encourage the patient to use Food First principles
- The powdered supplements are fully funded whereas the ready-made liquids are not. Full funding is available via "endorsement" for tube fed patients when using the ready-made liquids as a bolus tube feed.
- Is the patient lactose intolerant? Ensure Powder with water, and the ready-made liquids (Fortisip and Ensure Plus) are lactose free.
- Is the patient volume challenged? i.e. do they struggle to drink fluids at any volume? If so they should use a product which provides 1.5 kcal/mL.
- Measured volumes for mixing do not have to be exact, e.g 200 mL can be used instead of 196 mL. The key is to have the recommended amount of powder per day.
- Whilst there is a part charge for the ready-made liquid supplements, some patients may be willing to pay this especially if they prefer the taste and flavour varieties of the ready-made drinks or find it difficult to physically mix the powdered drinks or find the ready-made drinks convenient to carry when away from home.
- Is constipation an issue? Fortisip multifibre contains a mix of dietary fibres (4.6 g/200 mL) while the powdered drinks have a lower fibre content (Table 2).
Table 2: Nutritional composition of the ready-made and powdered drinks when mixed with water and milk
| Product | Mix | Vol(mL) | Kcal per serve | Kcal per mL | Protein per serve | Fibre per serve | Lactose | Subsidy |
| Powder drinks when mixed with water | ||||||||
| Ensure powder (can) | 6 scoops (53g)+ 195ml of water | 230mL | 230 | 1.0 | 8.5 | 2g | No | Full |
| Sustagen hospital formula (can) | 3 scoops (60g) + 200ml of water | 240ml | 228 | 1.0 | 13.8 | 0g | Yes | Full |
| Ensure powder (can) | 9 scoops (80g) + 180ml water | 230ml | 345 | 1.5 | 15 | 3g | No | Full |
| Powder drinks when mixed with 200ml of standard (blue top) milk | ||||||||
| Ensure powder (can) | 6 scoops (53g) | 230ml | 354 | 1.5 | 15 | 2g | Yes | Full |
| Sustagen hospital formula (can) | 3 scoops (57g) | 240ml | 352 | 1.5 | 20.3 | 0g | Yes | Full |
| Ready-made drinks | ||||||||
| Ensure plus (cans) | n/a | 237ml | 355 | 1.5 | 13 | 0g | No | Part |
| Ensure plus (tetrapak) | n/a | 200ml | 300 | 1.5 | 12.5 | 0g | No | Part |
| Fortisip (bottle) | n/a | 200ml | 300 | 1.5 | 12 | 0g | No | Part |
| Fortisip multifibre (bottle) | n/a | 200ml | 300 | 1.5 | 12 | 4.6g | No | Part |
| Two cal HN (can) | n/a | 237ml | 474 | 2.0 | 19.9 | 2.0g | No | Part |
Note: these instructions may vary from the mixing instructions on some of these products
Changing from ready-made liquids to a powder
When considering whether it is suitable for a patient to change from a ready-made liquid sip feed to a powdered sip feed the main considerations are; the purpose for which the patient needs the sip feed, the nutrient density of the sip feed, hidden costs and convenience.
Powdered sip feeds are not suitable for tube feeding. The ready-made sip feeds are fully subsidised where prescriptions are endorsed with "Bolus fed through a feeding tube". It is possible to also use fully subsidised tube feeding formula. Refer the patient to a dietitian for full review and recommendations.
Nutritional content
The ready-made liquid sip feeds, e.g. Ensure Plus and Fortisip, are 1.5 kcal/mL with 12 – 13g of protein per serve. In comparison, the powdered sip feeds (Ensure Powder and Sustagen Hospital Formula) when mixed with water according to the instructions provide 1.0 kcal/mL with 8.5 g and 13.8 g protein/serve respectively. By making a direct switch to standard dilution powdered drinks the nutrient density is reduced. This can be overcome if the powder is mixed with milk, the patient drinks a larger volume, or the powder is concentrated (refer to the mixing instructions in Table 2).
Tips for patients using powdered products
- Use the scoop provided so that the correct amount of powder is used
- Sustagen Hospital Formula and Ensure powder can be mixed with either water or milk
(preferably whole or full fat milk) - Mix using a spoon, fork, shaker, whisk or blender until the powder has dissolved – it may be easier to mix if the water/milk is added to the powder, rather than vice versa
Once mixed, it can be drunk straight away. Any leftover mixture can be covered and placed in the fridge for up to 24 hours. After 24 hours it should be thrown away.
Powdered products can be mixed with other food:
- Add other flavours, e.g. milkshake flavours, Milo, coffee or drinking chocolate
- Make a thick-shake by adding 2 teaspoons of instant pudding powder
- Make a hot drink by heating gently – but do not boil
Make a fruit smoothie by blending the made up mixture with:
- 1 banana and 2–3 tablespoons of ice cream or yoghurt
- ¼ cup of canned fruit and 2–3 tablespoons of ice cream or yoghurt
- ¼ cup of frozen berries
 Right click here, save target as... to download these tips in a PDF.
Right click here, save target as... to download these tips in a PDF.
Enteral feeding
In its broadest sense enteral nutrition refers to any feeding method that uses the gastrointestinal tract. More commonly, however, the term enteral feeding refers to methods of providing food via a tube directly into the gastrointestinal system.
The tube can be inserted through the nose to the stomach (nasogastric) or to the small intestine (nasoduodenal or nasojejeunal). Alternatively a feeding tube can be placed via the abdominal wall directly into the stomach (gastrostomy). Percutaenous Endoscopic Gastrostomy (or PEGs) refers to gastrostomy tubes that are placed using endoscopy.16
Enteral (tube) feeding should be considered for people who cannot eat and drink safely, such as with dysphagia following a stroke. It can also be used when people cannot maintain an adequate diet from normal food and fluids or from oral supplements.
If tube feeding is likely to be required for more than four weeks, then insertion of a PEG/gastrostomy tube may be required.16 The main benefit of gastrostomy tube over a nasogastric tube is patient comfort. It is also less likely to be displaced and can be hidden under clothes.1 However, a PEG is invasive and the risk of aspiration remains with both nasogastric and PEG feeding.24
NICE recommends that tube feeding in the community is delivered by health professionals trained in nutrition support using a coordinated multidisciplinary team approach.1 The team should include dietitians, district nursing, GPs and community pharmacists. Additional allied health staff should be involved as needed, e.g. speech and language therapists, occupational therapists. Monitoring of tolerance and oral intake by the team will provide guidance of when enteral feeding should be stopped.1
The use of tube feeding in people who are chronically unwell is controversial, especially when used for people with dementia. The debate focuses on the selection of which people will benefit from this form of nutritional supplementation.25 Both oral supplements and tube feeding can improve the nutritional state of people with dementia. European Society Parenteral and Enteral Nutrition (ESPEN) guidelines recommend that its use be considered in early and moderate dementia, however, not in terminal dementia.
The decision regarding the use of tube feeding must always be made on an individual basis with input from relatives, caregivers, GP, therapists and if required, legal representation.16
Considerations for the use of long-term tube feeding may include:16
- Does the patient suffer from a condition likely to benefit from enteral feeding?
- Will nutritional support improve outcome and/or accelerate recovery?
- Does the patient suffer from an incurable disease, but one in which quality of life and wellbeing can be maintained or improved by enteral nutrition?
- Does the anticipated benefit outweigh the potential risks?
- Does the use of enteral nutrition agree with the expressed or presumed will of the patient or in the case of incompetent patients of his/her legal representative?
- Are there sufficient resources available to manage enteral nutrition properly? If long-term enteral nutrition implies a different living situation, e.g. home vs institution, will the change benefit the patient overall?
Caution! Medicines and enteral feeds should not be mixed. Temporarily stop the tube feed flush with water, administer individual medicines, flushing the tube before and after each dose. Resume feeding.
Parenteral nutrition
Parenteral nutrition is a method of providing nutrition directly into the venous system, usually via a central line and so avoiding the digestive system. It is referred to as total parenteral nutrition and in general is used in a hospital setting. Its use in the community is mainly reserved for people with severe Crohn's disease, those with vascular damage to the bowel and some people with cancer. Home parenteral nutrition is expensive and requires careful patient selection and training and should be managed by a healthcare professionals trained in parenteral nutrition.
Acknowledgement
Thank you to Professor Tim Wilkinson, Associate Dean, Christchurch School of Medicine and Health Sciences, University of Otago and Dr Sandy McLeod, Medical Director, Nurse Maude Hospice, Christchurch, for expert guidance in developing the original article which appeared in BPJ 15 (Aug, 2008).
References
- National Institute for Health and Clinical Excellence (NICE). Nutritional support in adults. NICE, 2006.. Available from: www.nice.org.uk/Guidance/CG32 (Accessed Apr, 2011).
- Margetts BM, Thompson RL, Elia M, Jackson AA. Prevalence of risk of undernutrition is associated with poor health status in older people in the UK. Eur J Clin Nutr.2003;57:69-74.
- Milne AC, Potter J, Vivanti A, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev 2009;2CD003288.
- European Nutrition for Health Alliance (ENHA). Malnutrition among older people in the community: policy recommendations for change. ENHA,2006.. Available from: www.bapen.org.uk/pdfs (Accessed Apr, 2011).
- Watterson C, Fraser A, Banks M, et al. Evidence based guidelines for nutritional management of malnutrition in adult patients across the continuum of care. Dietitians Association of Australia, 2009.
- Babineau J, Villalon L, Laporte M, Payette H. Outcomes of screening and nutritional intervention among older adults in healthcare facilities. Can J Diet Pract Res 2008;69(2) 89-94.
- Pauly L, Stehle P, Volkert D. Nutritional situation of elderly nursing home residents. Z Gerontol Geriat. 2007;40:3-12.
- Chapman IP. Endocrinology of anorexia of ageing. Best Pract Res Clin Endocrinol Metab. 2004;18(3):437-52.
- Nowson C. Nutritional challenges for the elderly. NutrDiet 2007; 64(4):s150-S155.
- Pirlich M, Lochs H. Nutrition in the elderly. Best Pract Res Clin Gastroenterol 2001; 15(6): 869-84.
- Kaushal MV, Farrer K, Anderson ID. Nutritional support. Surgery (Oxford). 2008;26(2):54-9.
- Caro MMM, Laviano A, Pichard C. Nutritional intervention and quality of life in adult oncology patients. Clin Nutr 2007;26:289-301.
- van Bokhorst-de van der Schueren M. Nutritional support strategies for malnourished cancer patients. Eur J Oncol Nurs 2005;9(2):S74-S83.
- Barber MD, Fearon KCH. Should cancer patients with incurable disease receive parenteral or enteral nutritional support? Eur J Cancer 1998;34(3):279-82.
- Ash S, Campbell K, MacLaughlin H, et al. Evidence based guidelines for the nutritional management of chronic kidney disease. NutrDiet 2006:63 (Suppl.2):S35-S45.
- ESPEN Guidelines Group. ESPEN Guidelines on adult enteral nutrition. J Clin Nutr 2006;25(2).
- Feldblum I, German L, Castel H, , et al. Characteristics of undernourished older medical patients and the identification of predictors for undernutrition status. Nutr J2007;6:37.
- Hearing SX. Refeeding syndrome is underdiagnosed and undertreated, but treatable. BMJ 2004; 328(7445):908-9.
- Nitenberg G, Raynard B. Nutritional support of the cancer patient: issues and dilemmas. Crit Rev Oncol/Haematol 2000;34:137-168.
- Baldwin C, Weekes CE. Dietary advice for illness-related malnutrition in adults. Cochrane DatabaseSyst Rev 2009;1: CD002008.
- Dunne JL, Dahl WJ. A novel solution is needed to correct low nutrient intakes in elderly long-term care residents. Nutr Rev 2007;65(3):135-8.
- Stratton RJ, Elia M. A review of reviews: A new look at the evidence for oral nutritional supplements in clinical practice. Clin Nutr 2007;2(Suppl 1):5-23.
- Remsburg R, Sobel T, Cohen A, et al. Does a liquid supplement improve energy and protein consumption in nursing home residents ? Geriatr Nurs 2001;22(6):331-5.
- McMahon MM, Hurley DL, Kamath PS, Mueller PS. Medical and ethical aspects of long-term enteral tube feeding. Mayo Clin Proc. 2005;80(11):1461-76.
- Brotherton AM, Judd PA. Quality of life in adult tube feeding patients. J Hum Nutr Diet. 2007;20:513-22.
rollinsandelibubled.blogspot.com
Source: https://bpac.org.nz/bpj/2011/may/elderly.aspx
0 Response to "Ot Feeding Strategies in Elderly Population"
Post a Comment